COMPARING NORMAL, INTRAPERITONEAL AND SUBCUTANEOUS INSULIN DELIVERY
How Are They Different and Why Does It Matter?
How Are They Different and Why Does It Matter?
Clearly, the differences are considerable – but why is this important to those of us living with T1D?
Intraperitoneal Insulin Delivery is Closer to Normal: To begin with, intraperitoneal insulin delivery more closely mimics how insulin is delivered in a non-diabetic individual than subcutaneous insulin delivery does. This is not to say that IP insulin delivery is exactly the same as normal insulin delivery – just closer – in important ways.
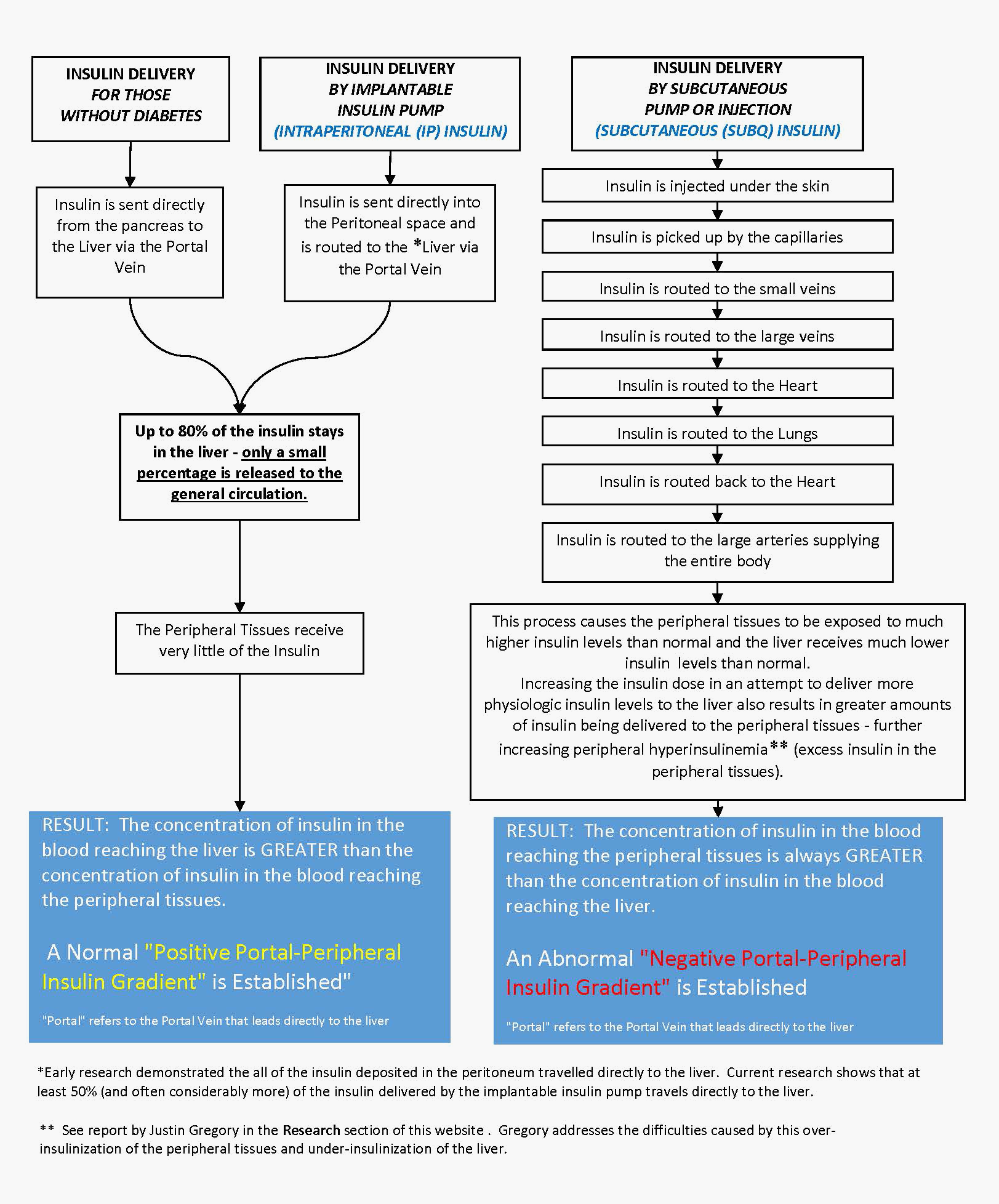
Intraperitoneal Insulin Delivery Supports the Liver’s Role in Controlling Blood Glucose: The liver plays a central role in maintaining a constant and appropriate level of blood sugar and to be able to do so the liver requires what is called a “Positive Portal-Peripheral Insulin Gradient”. A technical way of saying that the concentration of insulin in the blood that enters the liver needs to be greater than the concentration of insulin in the circulation of the rest of the body (the peripheral tissues). Intraperitoneal (IP) insulin delivery supports the maintenance of this Positive Portal-Peripheral Insulin Gradient while Subcutaneous (SubQ) insulin delivery does just the opposite and creates an abnormal Negative Portal-Peripheral Insulin Gradient where the insulin concentration reaching the liver is lower than the concentration of insulin in the rest of the body. This contributes to the difficulty of maintaining a stable blood glucose level experienced by those of us living with Type 1 Diabetes.
Intraperitoneal Insulin Delivery Makes Control More Possible Than Subcutaneous Insulin Delivery: A recent scientific publication* of a study led by Justin Gregory of Vanderbilt University School of Medicine points out the critical significance of this difference. This study examines the relationship between hypoglycemia in Type 1 Diabetes and two different routes of insulin delivery (peripheral, equating to subcutaneous insulin delivery and portal, equating to intraperitoneal insulin delivery). The concluding remarks of the paper are as follows. Note [Brackets added for clarity] Pe refers to peripheral insulin delivery and Po refers to portal (i.e. Liver) delivery. Emphasis has been added:
“The fact that insulin has to be delivered Pe [i.e., peripherally as in subcutaneous insulin delivery] clearly plays a role in causing hypoglycemia and glycemic variability. These studies suggest that strategies to mimic endogenous insulin secretion into the Po [i.e., the liver] circulation, such as intraperitoneal insulin delivery or use of hepatopreferential insulin analogs, should mitigate hypoglycemic risk and reduce fluctuations in glucose in patients with T1DM.”
Interestingly, this is exactly what the 450+ T1Ds who have an implantable insulin pump report! We find that it is easier to maintain a stable blood glucose level and hypoglycemia is less frequent and less severe than when we were receiving our insulin subcutaneously – and that is just part of the good news.
A more thorough description of Dr. Gregory’s research is included in our RESEARCH section of this website
*Diabetes, Volume 64, October 2015 Pages 3439-3451: Insulin Delivery Into the Peripheral Circulation: A Key Contributor to Hypoglycemia in Type 1 Diabetes