What Do We Know About The Implantable Insulin Pump and Intraperitoneal Insulin Delivery?
The T1Ds who have experienced Intraperitoneal Insulin Delivery and their doctors know that it is far more effective than Subcutaneous Insulin Delivery. An impressive statement – but what other evidence do we have to support their experiences? In fact there is quite a lot of evidence from research studies that extend from decades ago to the present time.
We have chosen a few research reports to highlight. Going forward, we will add summaries of other studies and if we receive specific topic requests for more information we will do our best to address them.
Summaries of a few of these research reports appear below. Some of the reports are from very recent studies and others from studies going back 30 years or more. The older studies are included show that we had considerable evidence of the superiority of intraperitoneal insulin delivery decades ago – far before it was possible to create an advanced implantable insulin pump!
Again, as we mentioned, we will be adding new examples of current and historical studies regularly and if we hear back from readers who want more information in any particular areas we will do our best to provide whatever information that is available to us.
Hypoglycemia: Subcutaneous Insulin Delivery Versus Intraperitoneal Insulin Delivery
There have been several published research reports that patients living with Type 1 Diabetes and who have an implantable insulin pump experience fewer and milder episodes of hypoglycemia than do patients receiving subcutaneous insulin (by injection or external insulin pump). The following, recent paper addresses this issue:
Insulin Delivery Into the Peripheral Circulation: A Key Contributor to Hypoglycemia in Type 1 Diabetes
Diabetes Volume 64:3439–3451, October 2015
Authors: Justin Gregory et al
In their Discussion section the authors state:
“The current study sought to determine the extent to which the route of insulin delivery influences susceptibility to hypoglycemia.”
This is a technical paper and requires careful reading – the essence of the paper, however, is summarized in the following statement: (Note bracket [ ] inserts are for clarification and are not included in the original)
“Current therapy in T1DM is further limited by the necessity of injecting insulin into subcutaneous tissue, which delivers insulin into the peripheral (Pe) circulation, rather than the hepatic portal (Po) circulation. This approach results in a reversal of the normal insulin distribution, with higher insulin concentrations in the Pe circulation [i.e., the peripheral circulation] and lower insulin levels in the hepatic portal Po circulation [i.e. circulation to the liver]. A therapeutic balance must therefore be achieved, such that the excess of insulin in the Pe circulation [i.e., the peripheral circulation] and its effect on glucose uptake offsets the deficit of insulin at the liver and its effect on glucose production. Because Pe overinsulinization [i.e., peripheral overinsulinization] shifts the primary site of insulin action away from the liver and toward skeletal muscle, a conceivable result is a predisposition to hypoglycemia.”
A somewhat less technical way of saying this is that in order to manage T1D with subcutaneous insulin it is necessary to deliver an excess amount of insulin in order to get enough insulin to the liver to help it regulate blood glucose. This over delivery of insulin acts upon skeletal muscle in a way that makes hypoglycemia more likely. In effect, trying harder to achieve excellent blood glucose control with subcutaneous insulin makes hypoglycemia more likely.
The concluding remarks of the paper are as:
“The fact that insulin has to be delivered Pe [i.e. subcutaneously] clearly plays a role in causing hypoglycemia and glycemic variability. These studies suggest that strategies to mimic endogenous insulin secretion into the Po [i.e., liver] circulation, such as intraperitoneal insulin delivery or use of hepatopreferential insulin analogs, should mitigate hypoglycemic risk and reduce fluctuations in glucose in patients with T1DM.”
Editor Comment: This is just what T1D implantable insulin pump users report. Hypoglycemia is less frequent, less severe, and far easier to recover from than it had been in the past when they were treated with subcutaneous insulin. They also report that maintaining a stable blood glucose is far more achievable and requires far less effort.
Intraperitoneal insulin administration in brittle diabetes
Published In: Brittle Diabetes. (Ed: Pickup,JC) Blackwell Scientific Publications, Oxford, 275-288, 1985
Authors: Schade, DS and Eaton, RP
This early experiment was performed in human diabetics who were experiencing difficulties with blood glucose control. The study was focused upon the physiology of intraperitoneal insulin delivery as compared to subcutaneous and intravenous insulin delivery. The delivery of insulin to the peritoneum was through the use of a percutaneous catheter inserted through the skin of the abdomen and into the peritoneal space. This is where implantable insulin pumps deliver insulin as well. At the time of this study implantable insulin pumps were not yet widely available for research purposes.
The authors report two interesting results First, in their Figure 21.5 below (from their 1985 publication) they showed that equivalent amounts of insulin delivered by intravenous, subcutaneous or intraperitoneal routes yielded very different peripheral insulin concentration profiles over a 4+ hour interval. It is clear that the intraperitoneal route resulted in the lowest peripheral exposure to insulin.
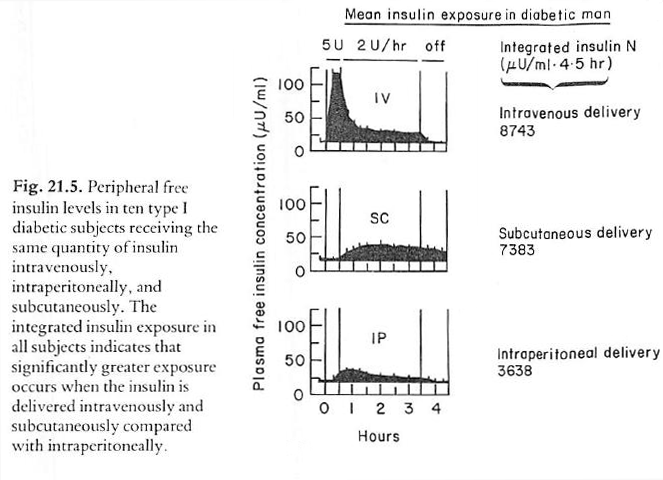
In a second portion of their study, Figure 21.15 below, that extended for 24 hours, the authors report normal peripheral insulin concentrations and glucose profiles with intraperitoneal insulin administration. Note: the title “Subcutaneous – peritoneal insulin injection” is a bit confusing. This was intraperitoneal insulin delivery through the use of a device implanted subcutaneously but delivering insulin to the peritoneum.
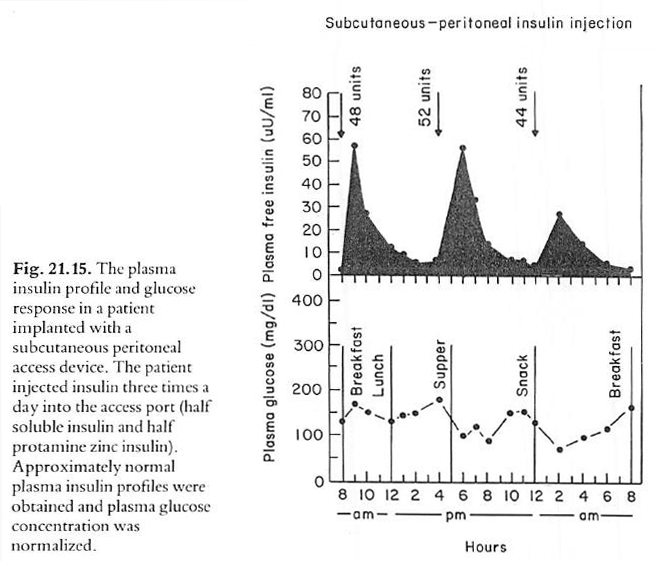
In summary, intraperitoneal insulin delivery normalizes peripheral insulin levels – thereby reversing the abnormal peripheral hyperinsulinemia seen with subcutaneous and intravenous insulin delivery.
Prolonged Peritoneal Insulin Infusion In Human Subjects
Prolonged peritoneal insulin infusion in a diabetic man.
Diabetes Care 3, 314. (1980)
Authors: Schade,DS; Eaton,RP; Friedman,NM; Spencer,W
In this five day study, the authors delivered insulin intraperitoneally through the use of a catheter that penetrated the abdominal wall and entered the peritoneal space. The results were similar to their other studies in that peripheral hyperinsulinemia was present with subcutaneous insulin delivery and was not present with intraperitoneal insulin delivery. There is far more area under the curve in the subcutaneous graph than in the peritoneal graph – demonstrating the hyperinsulinemia caused by subcutaneous insulin delivery.
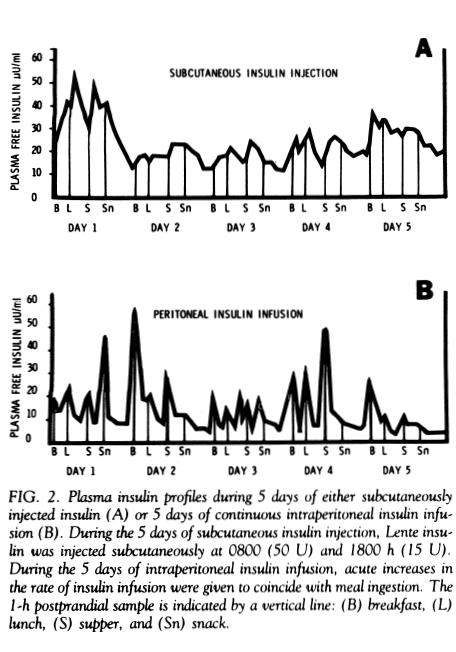
These early experiments, using what we would now consider unwieldy means of delivering intraperitoneal insulin, clearly demonstrated that intraperitoneal insulin delivery did not cause the peripheral hyperinsulinemia seen in subcutaneous insulin delivery. Not an unexpected result considering the normal behavior of the liver in extracting well over 50% of the insulin for its own use.
Clinical trial of programmable implantable insulin pump for type I diabetes: Effects on Hypoglycemia
Clinical trial of programmable implantable insulin pump for type I diabetes.
Authors: Selam,JL; Micossi,P; Dunn,FL; Nathan,DM
Diabetes Care 15(7), 877-885, (1992).
This study included 56 type 1 diabetic subjects who, prior to the study, were treated with either external insulin pumps (23 subjects) or multiple daily insulin injections (33 subjects). At the start of the study all patients had insulin pumps implanted (38 with insulin delivery to the peritoneum and 18 with intravenous insulin delivery to the superior vena cava).
Results: The incidence of severe hypoglycemic episodes for subjects with implantable insulin pumps was significantly reduced in comparison with the severe hypoglycemic episodes while these same subjects were receiving subcutaneous insulin.
| Treatment Details | Severe Hypoglycemic Episodes (episodes per patient year) |
| External Pump or Multiple Daily Injections | 0.47 |
| Implantable Insulin Pump | 0.05 |
As a comparison, the authors report that during the DCCT study the rate of severe hypoglycemia in the intensive control group was 0.74 episodes per patient year.
The authors conclude: To the contrary, and unexpectedly, we observed a striking decrease in the rate of severe hypoglycemia, with only 0.05 episodes of severe hypoglycemia per patient-yr compared with 0.47 episodes during the preimplant period and the rate of 0.74 episodes per patient-yr identified during intensive therapy in the DCCT. The absence of a random order assignment of intensive subcutaneous compared with intensive Implantable treatment in our study limits our confidence in concluding that implantable pump therapy is associated with a lower rate of severe hypoglycemia. Nevertheless, the 10-fold reduction in hypoglycemia frequency, with the same definition of severe hypoglycemia and careful prospective ascertainment as in the DCCT, is remarkable.
Note 1: Interpretation of these results is complicated by the mixture of delivery methods in the implantable pump phase of the study. The majority (68%) of implantable pumps delivered insulin to the peritoneum while 32% were delivering insulin intravenously. The mixture of delivery routes was common in early implantable pump studies since at that time, there was no common agreement on the optimal delivery route. Over time, the intraperitoneal route became the favored choice.
Note 2: The implantable insulin pump used in this study was the Infusaid Model 1000 which employed a unique infusion energy source that took advantage of the partial pressure of a special fluid within an enclosed space. Infusaid no longer offers implantable insulin pumps.
Insulin ---- Where It Is Delivered Is Really Important
This study, performed over 30 years ago (and if my research is accurate – based on the author’s work presented as early as 1967) dramatically illustrates the differences between the peripheral insulin delivery (similar to subcutaneous delivery) and portal insulin delivery (delivery to the liver).
Importance of Hepatic Portal Circulation for Insulin Action in Streptozotocin-Diabetic Rats Transplanted with Fetal Pancreases.
Authors: Brown, Mullen, Clark, Molnar & Heininger
Journal of Clinical Investigation. Volume 64 (Dec 1979), Pages 1688-1694
| Experiment Details | Result | |
| Step 1 | Rats are given the drug Streptozotocin (a drug that damages the insulin-producing beta cells of the pancreas). | All of the rats become diabetic. Blood sugars are over 500mg/ml and all show excessive urine formation. |
| Step 2 | Fetal pancreases from genetically identical rats are transplanted beneath the kidney capsule. | This placement results in insulin being sent to the general systemic circulation – approximating subcutaneous insulin delivery. Blood sugars and urine formation improve but are still significantly higher than normal. |
| Step 3 | A shunt is implanted that directs the insulin from the fetal pancreases to the liver. | Blood sugars dropped to normal levels and urine flow decreased to normal. |
| Step 4 | The shunt was removed – again sending insulin to the general systemic circulation. | Blood sugars and urine formation increase to greater than normal levels. |
From these results it is apparent that the manner in which insulin is delivered is very important. Delivering insulin to the liver (as is the normal situation when there is no diabetes) completely reverses diabetic symptoms in these animals, while delivering insulin to the general circulation, as subcutaneous insulin delivery does, improves the diabetic state but does not normalize it.
Figures 1 and 2 below have been extracted from the publication of this work:
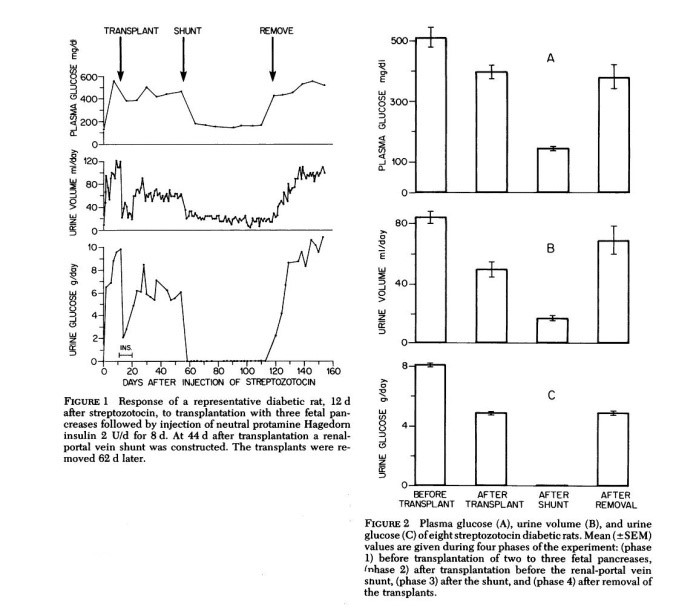
The authors conclude by stating:
“These studies demonstrate that shunting the venous drainage of pancreases transplanted under the kidney capsule from the inferior vena cava to the hepatic portal vein reverses to normal all measured parameters of the diabetic state. These include plasma glucose, the rate of glucose disappearance from blood after injection, and the IRI levels in blood before and after glucose injection. Urine volume and glucose content became normal and body weight gain increased.”
In other words, insulin delivered to mimic subcutaneous insulin delivery partially reversed the diabetic state but when that same insulin was directed to the liver (as it is in the normal state) the diabetes symptoms disappeared completely. Clearly, insulin works best when delivered to the liver.
COMING SOON: The Implantable Insulin Pump - The Foundation For A Superior Artificial Pancreas
An artificial pancreas, utilizing an implantable insulin pump that delivers insulin and measures glucose in the peritoneal space would have distinct advantages over a subcutaneous delivery and measurement system.
It has been established that the dynamics of insulin delivery and glucose measurement in the peritoneal space are faster and more reproducible than in the subcutaneous space – factors that greatly simplify the tasks of the control algorithm. There are additional factors as well that show the superiority of intraperitoneal insulin delivery and intraperitoneal glucose measurement.
This topic is of current importance for at least three reasons:
- There is a high level of interest within the diabetes community regarding the artificial pancreas.
- The advantages of an intrperitoneally based artificial pancreas are considerable. We need we urgently need to bring this to the attention of our community
- Although the physiological superiority of an intraperitoneal system are clear the implantable insulin pump has not been developed using the current technological capabilities that are now available. There is a clear need to accelerate the development of such a system.
We will be developing this section and posting relative research summaries in the weeks to come.
COMING SOON: Is there evidence that intraperitoneal insulin deliery has positive effects beyond glucose control?
The short answer is Yes.
We will select a series of research articles that address this question and begin posting them in January 2017 (perhaps earlier, time permitting).